Education
Station
Understanding Oral Microbiome's Impact on Periodontal Disease
The mouth’s degradation typically happens in three ways: tooth decay, periodontal disease (affecting gums and bones), and mechanical dysfunction. The initial two forms of decay arise from an imbalance in the oral microbiome, much like how an imbalance in gut bacteria can lead to health issues. The oral cavity is abundant with diverse bacteria, both beneficial and harmful, living in harmony referred to as symbiosis. When harmful bacteria overgrow, outnumbering the beneficial ones, a condition called dysbiosis arises. Dysbiosis can lead to complex conditions impacting different tissues, due to the unique and distinctive microcolonies and biofilms formed by the bacteria.
For example, while multiple bacteria are involved, Streptococcus mutans is the main strain causing tooth decay. This bacteria thrives in the deep crevices on the posterior teeth's chewing surfaces, between teeth, and the gum/tooth interface. These bacteria consume carbohydrates, especially simple sugars including fruits, and excrete acid, dissolving the enamel, leading to tooth decay. Periodontal disease arises from more intricate biofilms beneath the gums. Both direct bacterial actions and indirect host (immune) reactions result in the disease's progression. Saliva is a major defense against periodontal disease, and alterations in salivary flow or components can aid harmful biofilms' growth. Several local and systemic factors contribute to periodontal disease, including:
- Poor oral hygiene
- An unhealthy diet (rich in sugars and processed foods)
- Stress
- Misaligned or crowded teeth
- Immune deficiencies
- Genetic mutations
- Toxins disrupting normal immune response or tissue/bone turnover
- Gut dysbiosis
- Mouth breathing
- Faulty or deteriorating dental work
- Dry mouth (side effects of medication; autoimmune disorders)
- Hormonal fluctuations (especially during pregnancy)
- Oral contraceptives
- Smoking
- Diabetes
Traditionally, periodontal disease is diagnosed through intra-oral evaluation, x-rays, periodontal charting, and observing longitudinal results. This method can lead to delayed detection, during which silent damage can occur. In contrast, modern DNA techniques enable us to sample the oral microbiome and detect changes before chronic disease establishes a firm grip.
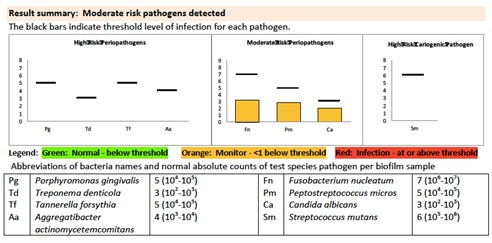
The below examples illustrate bacterial DNA test results from two different patients. The first patient's results raise concerns, showing high levels of "moderate risk" bacteria and moderate levels of "high risk" (more destructive) bacteria. This pattern is not common and most challenging to treat. Alongside an intensive oral regimen, systemic issues contributing to this oral condition need addressing, requiring consultation with an integrative health practitioner, functional medicine doctor, or naturopath.
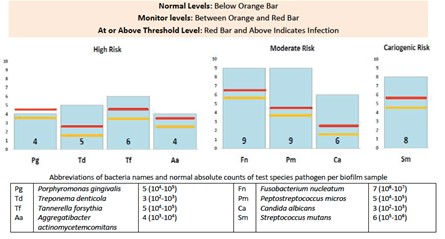
The following results represent a milder stage of periodontal disease. Correcting this condition might require less extensive interventions such as diet modification, improved oral hygiene, increased cleaning frequency, and introduction of new hygiene products.
Regardless of the treatment modality, the key to successfully managing periodontal disease lies in achieving a balanced oral microbiome and a robust immune response. This implies addressing both local and systemic contributing factors.
Managing Periodontal Pathogens
The first step towards a disease-free mouth involves reducing harmful bacteria and fostering beneficial ones. Long-term use of non-selective antibacterial products, which eliminate both good and bad bacteria, is discouraged. This includes alcohol or Chlorhexidine-containing mouthwashes and toothpastes with fluoride, foaming agents, or other chemicals. Our protocol promotes ozone and potent anti-inflammatory and antibacterial plant extracts, combined with mechanical debridement and followed by oral probiotics. For home care, we recommend natural oral products to maintain a balanced oral microbiome.
Dietary Changes
Restoring oral health first involves evaluating and potentially altering your diet, mainly avoiding sugars (particularly added sugars found in many foods), highly processed foods, frequent snacking, and carbonated drinks (which acidify the mouth).
Oral Hygiene
The goal is to disrupt the biofilm forming between the teeth, below the gums, and on the tooth root surfaces. Brushing and flossing at least twice daily is essential, and using a WaterPik morning and night can be effective. Adding natural mouthwashes and certain oils, like grapefruit seed extract, and grape seed extract, known to kill harmful bacteria, can be beneficial. The use of Proxabrushes or Soft-Picks is also highly recommended. We suggest several other beneficial products to our patients.
Mechanical Debridement
The cornerstone of all periodontal therapy is scaling and root planing (“deep cleaning”), which mechanically removes the calcified biofilm beneath the gums. The number and frequency of these sessions depend on your specific microbiome.
Ozone Rinses
BioSure offers high-quality home products that can create ozone water in just three minutes using tap water. Ozone, an antioxidant form of oxygen, effectively kills bacteria, viruses, and fungi and is entirely safe with zero side effects.
Probiotic Lozenge
Following the antibacterial rinse regimen, beneficial bacteria should be introduced via oral probiotic lozenges, either Great Oral Health or Hyperbiotics Pro-Dental, used indefinitely.
Re-testing
Re-testing is crucial for understanding individual responses to treatment. Achieving complete resolution is not the aim but rather making progress as periodontal disease is chronic and requires dedicated efforts from both you and our dental team. Ensuring no disease relapse via periodic re-testing (every 1-3 years) is recommended. If the disease recurs despite addressing all local factors and adherence to our advice, systemic factors might be involved. In this case, we highly recommend you consult with an integrative or functional health practitioner for a comprehensive cellular-level health evaluation, to identify any other toxins, hidden infections, or genetic abnormalities interfering with your immune response.
The Oral/Systemic Connection
Previously, bacteria associated with periodontal disease were thought to be confined to the mouth. Now, substantial evidence supports the notion that these bacteria can enter the bloodstream, traveling to other body parts, and causing disease at distant sites. Therefore, we recommend a relationship with an integrative or functional health practitioner, who can evaluate your health on a cellular level, as well as the gut microbiome.
Our Pledge
We consistently strive to evolve our treatment recommendations based on the latest research. If newer treatment options emerge fitting our health-oriented approach, you will be informed. We value patient education about their current health state, the ideal health state, available treatment options, and the risks and benefits of those options. Your questions are always welcome; reach out to LeBlanc Dental today via phone or email to learn more about holistic dental care.
Sincerely,
LeBlanc Dental
- Seymour T, Zhang J. Porphyromonas Gingivalis in the Pathogenesis of Alzheimer’s Disease and Its Therapeutic Target. Journal of Exploratory Research in Pharmacology 2022;7(1):45-53
- Zhang J, Xie M, Huang X, Chen G, Yin Y, Lu X, Feng G, Yu R, Chen L. The Effects of Porphyromonas gingivalis on Atherosclerosis-Related Cells. Front Immunol. 2021 Dec 23;12:766560. doi: 10.3389/fimmu.2021.766560. PMID: 35003080; PMCID: PMC8734595.
- Ni Wang, Jing-Yuan Fang, Fusobacterium nucleatum, a key pathogenic factor and microbial biomarker for colorectal cancer. Trends in Microbiology, Volume 31, Issue 2, 2023, Pages 159-172.